.......
![[圖]](https://i.imgur.com/6yPzoQb.jpg)
![[圖]](https://i.imgur.com/U8YMSVj.jpg)
![[圖]](http://img.medscape.com/slide/migrated/editorial/cmecircle/2006/6095/images/figure4.jpg)
Understanding migraine
Introduction
As pharmacists, we are uniquely positioned to helpmigraine patients receive a proper diagnosis of their condition and be treated appropriately and effectively. Discussions about headache between pharmacist and patient are extremely frequent: according to large-scale surveys, pharmacists recommend headache products about 53,000 times a day on average in the United States.[url=javascript:newshowcontent(][1][/url] Additionally, pharmacists are key learned intermediaries for undiagnosed, misdiagnosed, or inadequately treated headache patients, many of whom choose not to seek a physician's care. We are also important educational sources for diagnosed migraine patients, especially about their prescription medications.
Furthermore, headache is still poorly understood, even though it is the most common form of human pain. As educators, we can help correct many of the myths that persist about migraine among the patient population: these myths often prevent a patient from seeking medical treatment and are barriers to effective care.
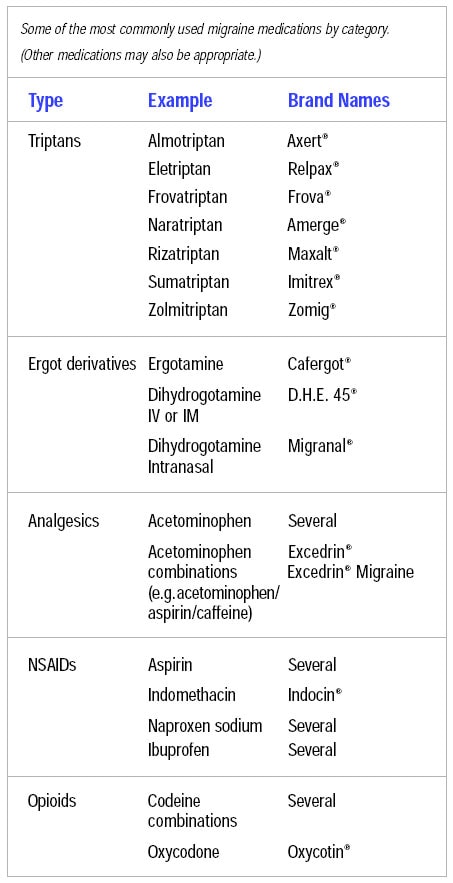
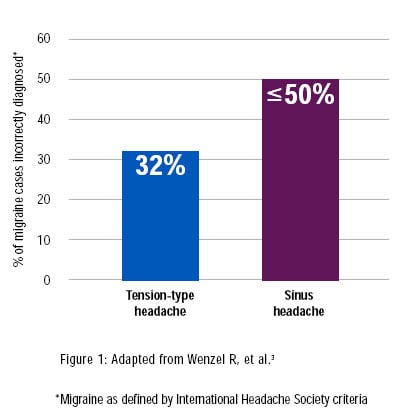
migraine Myths
migraine is neither an "extreme headache" nor a psychosomatic condition, as many patients and some healthcare providers continue to believe. One of the most pervasive misconceptions is that migraine is a vascular disease. Current and emerging evidence disproves this notion and has established that migraine has a distinctive physiology based on a neurological process. Due to poor understanding about the condition, migraine is often misdiagnosed – or not diagnosed at all. It is frequently mistaken for tension-type or sinus headache, even though headache specialists consider the latter to be relatively rare.[url=javascript:newshowcontent(][2][/url]
[url=javascript:showslide(]
 [/url][url=javascript:showslide(](Enlarge Slide)[/url]
[/url][url=javascript:showslide(](Enlarge Slide)[/url]Prevalence and Epidemiology
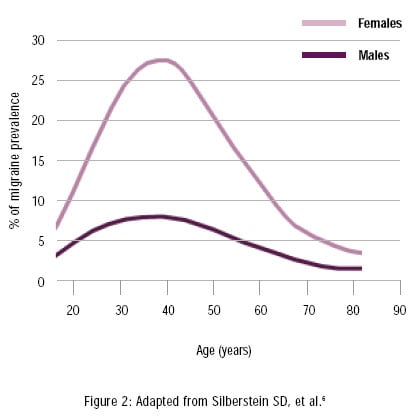
migraine is a common disorder in the United States. The National Headache Foundation reports that about 29.5 million Americans are affected and as many as half remain undiagnosed.[url=javascript:newshowcontent(][3][/url] Before puberty, the prevalence of migraine is similar in boys and girls. However, post puberty, migraine becomes increasingly common in women, at a rate that is 2.5 to 3 times higher than in men.[url=javascript:newshowcontent(][4][/url] The preponderance in women, which persists throughout adulthood, may be related in part to hormonal factors.[url=javascript:newshowcontent(][4][/url] However, since the gender disparity continues beyond menopause, other factors must be involved, yet are not well understood.[url=javascript:newshowcontent(][4][/url] Age is also a factor, with incidence rates increasing after age 12 and peaking at approximately age 40.[url=javascript:newshowcontent(][4,5][/url]
Pharmacist Fact
migraine patients make up one third or more of a pharmacy's customers, according to 45% of pharmacists.[url=javascript:newshowcontent(][1][/url]
The American migraine Study II has documented the extent of migraine on the American family: as many as 1 in every 4 households has a migraine sufferer. More than half of migraine sufferers have not sought a medical diagnosis.[url=javascript:newshowcontent(][5][/url] No matter how debilitating their symptoms, many patients view migraine as a character flaw or an inability to handle stress.
[url=javascript:showslide(]
 [/url][url=javascript:showslide(](Enlarge Slide)[/url]
[/url][url=javascript:showslide(](Enlarge Slide)[/url]Impact of migraine
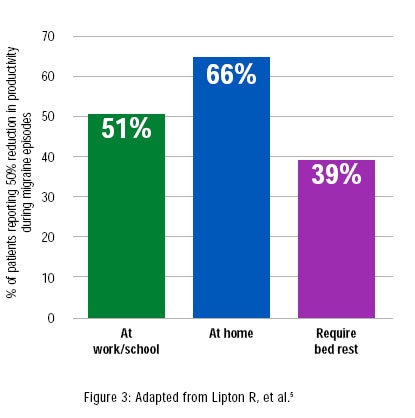
migraine causes significant disability, affecting home life, work, and social activities. It is associated with extensive deterioration in the quality of life. More than 6 of 10 diagnosed patients have reported that their migraine episodes leave them severely impaired,[url=javascript:newshowcontent(][5][/url] while more than 9 of 10 report at least some headache-related disability.[url=javascript:newshowcontent(][7][/url]
Other population-based studies have reported that 45% of migraineurs say they are forced to miss family social and leisure activities, while 32% avoid making plans for fear of cancellation due to headaches.[url=javascript:newshowcontent(][8][/url] About 50% of people with migraine believe that, during their migraines, they are more likely to argue with their spouse or their children, and up to 73% feel their migraines adversely affect their relationships with their families and work colleagues.[url=javascript:newshowcontent(][8][/url] Partners who participated in the studies confirmed these findings: up to 60% reported negative effects at home because of the other person's headaches.[url=javascript:newshowcontent(][8][/url]
The economic impact of migraine is severe, with direct and indirect costs amounting to billions of dollars a year in the United States alone. In a 2005 review, one researcher noted that the estimated annual costs of migraine and its treatment total as much as $17 billion dollars.[url=javascript:newshowcontent(][9][/url] Direct costs include over-the-counter and prescription medications, physician office visits, diagnostics, emergency room visits, and hospitalization. Indirect costs included lost productivity and absenteeism. It has been estimated that at least 150 million workdays are lost each year due to headaches.[url=javascript:newshowcontent(][10][/url]
"The burden of migraine stretches beyond just patients to family members, employers, and society as a whole" Wenzel R, et al
11
[url=javascript:showslide(]
 [/url][url=javascript:showslide(](Enlarge Slide)[/url]
[/url][url=javascript:showslide(](Enlarge Slide)[/url][url=javascript:showslide(]
 [/url][url=javascript:showslide(](Enlarge Slide)[/url]
[/url][url=javascript:showslide(](Enlarge Slide)[/url]Diagnosis and Pathophysiology of migraine
Symptoms
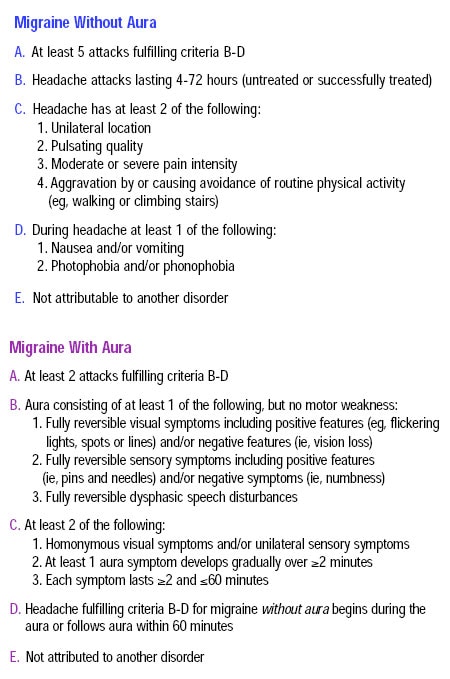
According to symptoms-based International Headache Society (IHS) diagnostic criteria, migraine is usually (although not always) associated with moderate-to-severe head pain.
In contrast to tension-type headaches, which tend to be bilateral and constant, migraine is predominantly unilateral in pain location and throbbing.[url=javascript:newshowcontent(][11][/url] Some of the symptoms of these 2 headache types overlap – for instance, migraine pain may occasionally present as bilateral and constant. However, migraine can usually be distinguished by the fact that associated pain is aggravated by routine activity.[url=javascript:newshowcontent(][11][/url] migraine can be associated with gastrointestinal distress and with certain sensory disturbances, such as aura.
Current pathophysiologic understanding[url=javascript:newshowcontent(][12][/url]
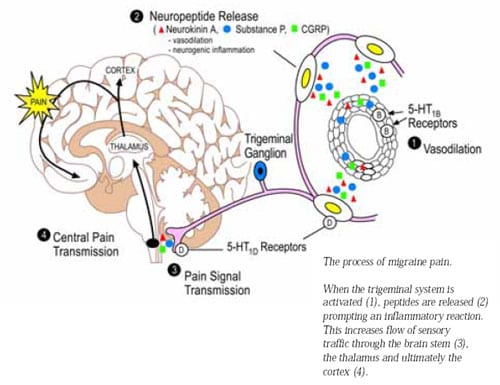
migraine is now known to be a neurological process of the trigeminovascular system, rather than a vascular event. The vascular theory has been debunked for several reasons:
- vascular changes do not explain the premonitory and other symptoms linked with migraine.
- some useful migraine treatments have little effect on vasculature.
- according to blood flow studies, vascular changes only occur randomly in migraine attacks and do not correlate with the clinical features of the condition.
migraine is a neurochemical chain reaction that involves 5 distinct phases of a neurological process: prodrome, aura (may or may not be present), mild, moderate, or severe pain, and postdrome.
Once the reaction is "triggered" (see causes in next section), fluctuation in neuronal activity may activate the trigeminovascular system in the meninges. Once activated, the trigeminal afferent can release various vasoactive peptides, producing an inflammatory response that probably causes head pain.
In turn, the inflammatory response lowers the sensory threshold of the trigeminal afferents, increasing the flow of sensory traffic to the second-order neurons in the brainstem, especially the trigeminal nucleus caudalis. The sensory material is allowed to reach high centers of the thalamus and cerebral cortex – the central areas of pain perception.
migraine symptoms follow the escalating neuronal process. migraine attacks tend to build in pain intensity and frequency over hours or days. The activation of the trigeminal system also explains facial pain and neck pain that can occur during migraine and that are often mistaken for symptoms of either a sinus or tension-type headache.
Up to 20% of all migraine patients present with aura. It is believed that this is caused by cortical spreading depression with extensive glutamate release.[url=javascript:newshowcontent(][12][/url]
[url=javascript:showslide(]
 [/url][url=javascript:showslide(](Enlarge Slide)[/url]
[/url][url=javascript:showslide(](Enlarge Slide)[/url][url=javascript:showslide(]
 [/url][url=javascript:showslide(](Enlarge Slide)[/url]
[/url][url=javascript:showslide(](Enlarge Slide)[/url]Common precipitating factors
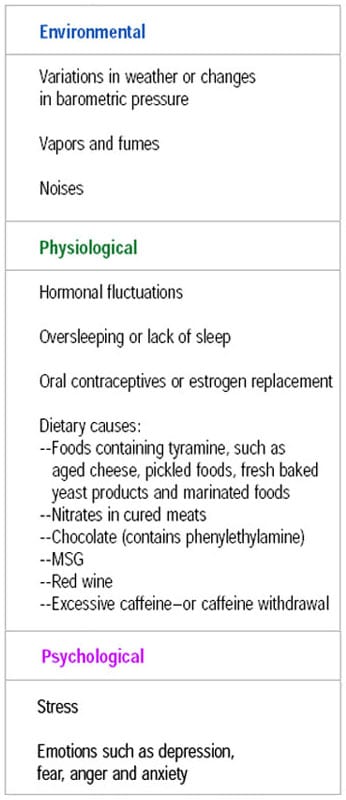
The precipitating factors involved in migraine are commonly known as "triggers" and are generally associated with environmental or external stimuli or with either physiological or psychological parameters.
The Pharmacist's Role
Suggest that headache patients keep a "diary" as a record of when their episodes occur. They should also record the frequency, duration, and severity of their attacks. This will help their physician diagnose their condition and also help identify their triggers. You can find an example of a diary at the National Headache Foundation Web site, www.headaches.org
Treatment Options
Due to increased scientific understanding, the clinical treatment of migraine has advanced considerably over the last 20 years. Today, it is possible for migraine to be accurately diagnosed and effectively managed. Successful management includes a number of factors: appropriate use of medications, elimination of precipitating causes, routine monitoring and follow-up, and patient education.
Treatment is dependent on the individual's history. For instance, because severely nauseated or vomiting patients do not absorb oral medications, nasal sprays or injections are more likely to be effective. migraine treatments fall into 2 categories: acute or preventive.
Acute treatment
Acute treatments stop a migraine attack that is in progress. These medications tend to work better if taken early in the attack. Acute, or abortive, therapies are indicated for those patients who experience occasional migraines. Ideally, such a patient will have 2 acute agents on hand: one as their drug of choice and the other to use when their first choice fails, which can happen from time to time.
Over-the-counter analgesics can help individuals with mild to moderate attacks. Research demonstrates that migraine-specific medications, including triptans and dihydroergotamine, are the most effective agents for moderate to severe attacks. Triptans are available in oral, self-dissolving tablets, nasal, and injectable formulations (please see Table 6), while dihydroergotamine is marketed as an injection and nasal spray.
Antiemetics can be combined with migraine-specific drugs in patients with significant gastrointestinal symptoms.
As a general rule, patients who have received an acute agent need to treat 3 attacks with it to determine efficacy. If the drug fails to provide relief in at least 2 attacks, the patient should be switched to another acute agent. Patients who fail multiple acute agents or who use their acute medication more than 3 days a week should be referred to a headache specialist.
Preventive treatment
Preventive, or prophylactic, treatments are used when migraine headaches occur frequently or are debilitating. These treatments can be used episodically in certain conditions (such as unavoidable exposure to a trigger) or long term. Many effective preventive treatments are available. In a large study, the American migraine Prevalence and Prevention Study (AMPP), conducted in 2004 and presented in 2005, it was found that 12% of Americans have migraines and approximately 40% could benefit from preventive therapies, while only 1 (20%) in 5 currently use prevention therapy.[url=javascript:newshowcontent(][15][/url]
※ 編輯: ott 時間: 2019-06-20 15:38:41